Page Contents
Sleep is essential for our mood, memory and metabolism. It impacts on every part of our lives and when we don’t get enough it can impact on both our physical and mental wellbeing. Sleep deprivation can also lead to weight gain and puts us more at risk of things like sleep apnoea.
There is no disputing that sleep is fundamental to our health and wellbeing.
It has been found that up to 40% of patients who have post Covid syndrome (long COVID) symptoms are struggling with their sleep, this could be a new or exacerbated sleep difficulty following Covid infection.
Why this is more prevalent following Covid infection remains unclear although it is completely normal to sleep more during infection and for some, it might be difficult to get back into their normal sleep routine. Some medications cause sleep disturbances too. Being indoors more and not being exposed to natural daylight can also cause disruption to our circadian rhythm (or body clock). Sleep disturbances can also be caused by low mood and anxiety. If you are concerned please do speak to your GP. There are also some helpline numbers at the bottom of this page.
Types of Sleep Difficulties
Sleep difficulties can take the form of delayed sleep onset (lying in bed for more than 15 -20 minutes and struggling to get off to sleep), waking up during the night and struggling to get back to sleep for some time afterwards, you might also wake up too early in the morning. It could of course, be any combination of these.
Understanding the brain/body connection for sleep
Understanding the mechanisms relating to sleep can help to understand what is happening and give you more insight into things that you can put in place to help achieve better sleep.
What happens when we are asleep?
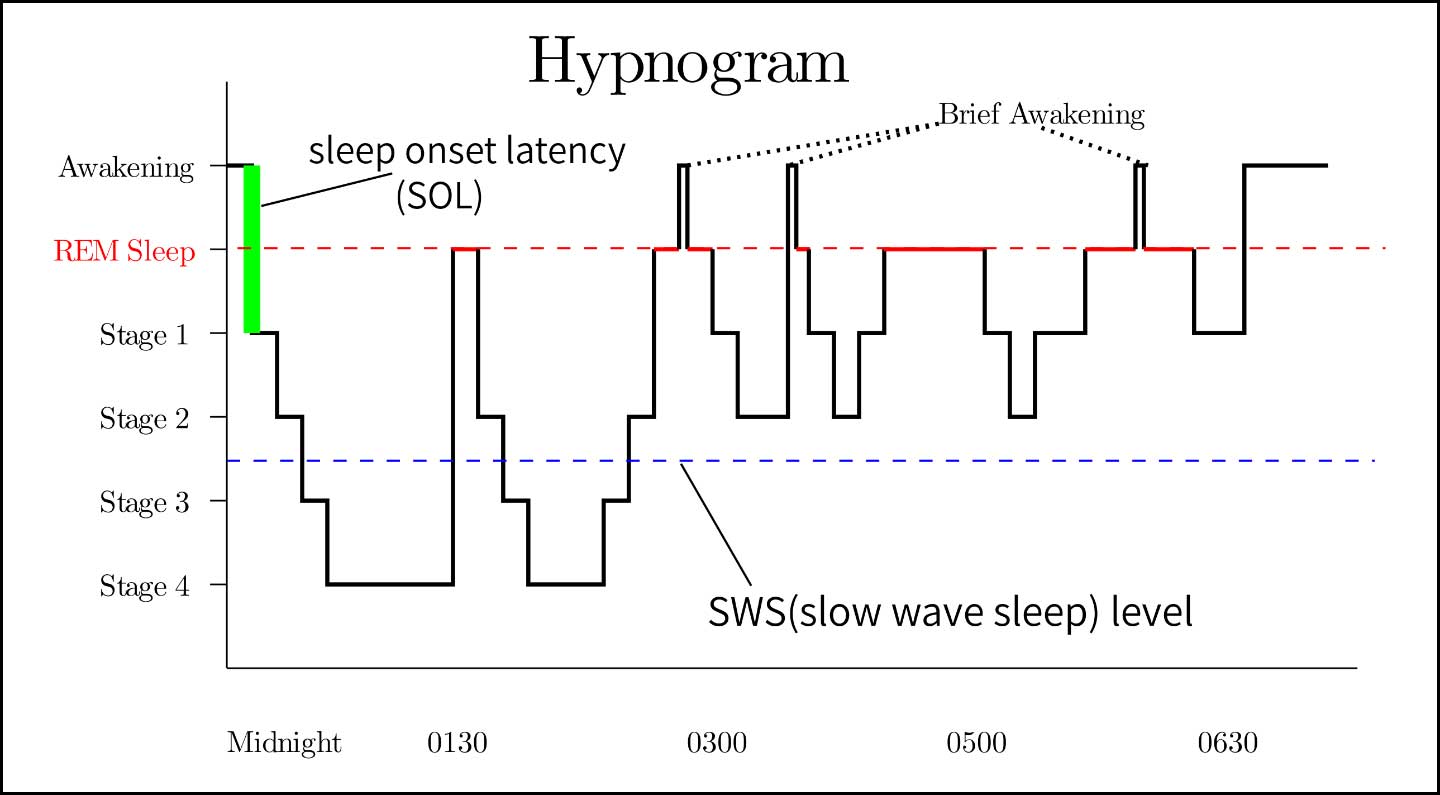
When you fall asleep at night you cycle through a number of stages – these are known as sleep stages. A typical sleep cycle in an adult lasts around 90 minutes and depending on your total sleep duration, you may have several of these during the night.
What makes up a sleep cycle?
It is completely normal to wake up during the night although for many people they are not aware. It is how you respond to the night wakening which counts.
What governs sleep?
Scientists call this ‘sleep homeostasis’ but we can refer to this as our sleep drive.
In principle, the longer we are awake the more our sleep drive builds – similar to how hunger slowly builds after a meal.
Usually when we have been awake for around 16 hours our sleep drive should be at its richest. But like hunger, we know if we snack between meals we may not be as hungry at our next meal, naps can also affect sleep pressure. A short nap up to 20 minutes does not appear to affect sleep pressure and some people find naps beneficial.
As human beings we also have something known as a circadian rhythm or sleep/wake cycle.
We are governed by night and day over a 24 hour period. There is a group of cells within the brain called the suprachiasmatic nucleus (SCN) that control when we feel sleepy and when we feel alert. You might find that you are more sleepy in the afternoon and this is due to a natural peak in the mid-afternoon of this sleep/wake cycle.
What helps achieve better sleep?
You may have heard of something called Sleep Hygiene? – this is nothing to do with cleanliness but refers to creating a routine and an environment which is sleep friendly.
Here are some suggestions but you can find more on the Your COVID Recovery website.
Bedroom Environment
- Check your bedroom temperature – is it too warm or too cold? The temperature should be around 16-18 °C /60-65 °F. Your bedroom should be dark and quiet (blackout curtains are very helpful, particularly in the summer months).
- Try to keep your bedroom as a place for sleep – avoid watching TV, working, gaming etc in the bedroom.
- Clear your bedroom of clocks – checking them helps your brain to keep more accurate track of time and is not helpful for regular night waking. Keeping check of the time can cause you to worry that you only have a certain number of hours left to sleep so try not to look at the time when you are trying to sleep.
Routine/Behaviours
- Sleep/wake cycle, as mentioned above, is governed by our 24 hour circadian rhythm. Try to keep to a regular wake time and ensure as much natural daylight as possible as soon as you can after waking.
- Caffeine is a stimulant and can mask the build-up of sleep drive – some people are more sensitive to the effects than others but it’s worth bearing in mind that caffeine has a half-life of 5-7 hours (this means that half of the chemicals from caffeine have left your body in this time). It is also worth noting that caffeine is not just present in coffee or tea, many painkillers, soft drinks and dark chocolate also contain a level of caffeine.
- Alcohol may help people to fall asleep quicker, but it is better to avoid or cut down before bedtime. Alcohol is broken down very quicky by the body and during the second half of the night it can cause frequent early morning waking – it can also stop people from entering into REM sleep which can lead to a number of health problems. Of course, having a lot to drink also can cause more visits to the loo and drinking on a regular basis can lead to an alcohol dependency. It is not sleep’s friend.
- Nicotine, like caffeine is a stimulant which can disrupt sleep, it can also make restless legs much worse. If you do smoke, try to think about quitting all together, the health benefits are huge. If you aren’t able to do this right now, try to have you last cigarette 2 hours before you plan to go to bed.
- Exercise can be good for sleep but please ensure that you have checked with the Long Covid clinic before embarking on any high-intensity (exercise that makes you out of breath) before carrying out any exercise programme. If you do any exercise try and keep this away from bedtime (at least 4 hours before) otherwise it can stop you from getting to sleep.
- Technology – avoid looking at bright screens for at least the last 30 minutes before bed. The blue light omitted from screens (mobiles, TVs & tablets) can all stimulate your brain into thinking it is still daytime.
- Although you might feel fatigued with Long Covid, do not go to bed until you feel tired enough to sleep. If you find that you are lying in bed for more than 15-20 minutes, as hard as it may feel, get out of the bedroom and do a non-stimulating activity in a dim room. This could be reading but adult colouring books and jigsaws have been found to help too. Only return to your bed when you feel tired enough to sleep.
There are also sleep mediations which can help soothe a busy mind. Once learnt you can replicate without any technology once in bed. Here are some examples:
Progressive-Muscle-Relaxation.mp3
For further information
The Sleep Charity has a dedicated website to help adults with their sleep:
You can also find more information from the NHS to help with sleep difficulties.
If you are concerned about your mood, please talk to your GP. Your GP is best placed to support you and point you in the direction of helpful services.
If you feel that you need more urgent help or it is out-of-hours, then you can access the following sources of support:
- Life-threatening situation – If you or a loved one are in a critical or life-threatening situation (this includes risk of harm to self) you should call 999 straight away.
- NHS 111 Option 2 is a helpline for people of all ages who need urgent mental health support. The helpline is available all day, every day. Telephone the helpline on 111 and select option 2 if you are feeling unsafe, distressed or worried about your mental health.
Derbyshire Mental Health Helpline and Support Service
0800 028 0077
“The Derbyshire Mental Health Helpline and Support Service is a freephone service available to everyone living in Derbyshire – both young people and adults. It is open 24 hours a day, seven days a week. If you or your loved one are experiencing distress or anxiety, or feeling that you cannot cope, call us on 0800 028 0077 for support over the phone. That support could be about your mental health but you can also talk through practical issues that may be causing concern.”
Samaritans
116123
Or email: jo@samaritans.org
CALM
0800 58 58 58
Aimed particularly at men. “Our helpline is for people in the UK who are down or have hit a wall for any reason, who need to talk or find information and support”.
Papyrus
HOPELINEUK: 08000684141
Text: 07860 039967
Email: pat@papyrus-uk.org
For young people: “We provide confidential support and advice to young people struggling with thoughts of suicide, and anyone worried about a young person”
Mind
Mind has a list of ways to help yourself cope in a crisis
SANEline
0300 304 7000
Saneline is an out-of-hours telephone helpline offering practical information, crisis care and emotional support to anybody affected by mental health problems. They also provide a free text-based support service called Textcare (see their website). Available between 4.30pm – 10.30pm each evening, every day of the year.
The Silver Line
0800 4 70 80 90
Aimed at people over 55. Their helpline is open 24 hours a day, every day of the year.
The Mix
0808 808 4994
Aimed at people under 25. Their helpline is open between 4pm and 11pm, 7 days a week. They also run a crisis text service which is open 24 hours a day, 7 days a week. Text THEMIX to 85258
Webchat: through the website. (4pm – 11pm, 7 days a week)
Apps for your Smartphone which you might find helpful
Calm Harm
A great resource for helping people ‘ride the wave’ of emotional distress.
Stay Alive
“This app is a pocket suicide prevention resource packed full of useful information and tools to help you stay safe in crisis. You can use it if you are having thoughts of suicide or if you are concerned about someone else who may be considering suicide.”
Other organisations that you might find helpful:
Rethink Derbyshire Recovery and Peer Support Service
01773 734989
“We support people who are having difficulties with their mental health across the whole spectrum of mental illnesses. We do this by offering targeted goal-focused support, developing peer support and volunteer opportunities across Derbyshire, and also peer support groups where there is a need”
You can self-refer or ask a health professional to refer you.
Op COURAGE: the Veterans Mental Health and Wellbeing Service
0300 323 0137 or email mevs.mhm@nhs.net
Op COURAGE is an NHS mental health specialist service designed to help serving personnel due to leave the military, reservists, armed forces veterans and their families.
